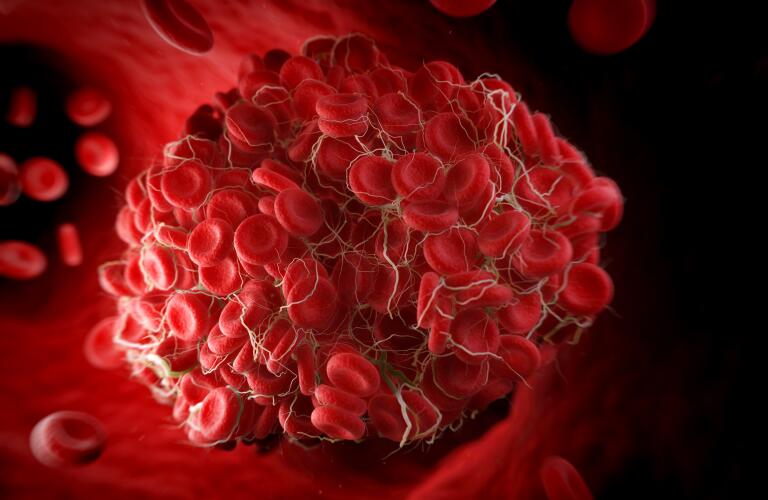
COVID-19 and blood clot: A blood clot is a clump of blood that has changed from a liquid to a gel-like or semisolid state. Clotting is a necessary process that can prevent you from losing too much blood in certain instances, such as when you’re injured or cut. When a clot forms inside one of your veins, it won’t always dissolve on its own.
COVID-19 is an illness that’s caused by the new coronavirus, SARS-CoV-2. Many symptoms of COVID-19, such as cough and shortness of breath, affect your respiratory system.
However, the virus can also have other effects on your body. For instance, in some cases it can cause gastrointestinal symptoms, loss of smell or taste, or even a toe rash.

Another possible side effect of COVID-19 is that it can lead to blood clots in some people.
COVID-19 and blood clots
- Causes
- Risk factors
- Complications
- Treatment
- Blood clot prevention
- Bottom line
In this article, we’ll take a closer look at how COVID-19 can contribute to the formation of blood clots, who’s at higher risk, and the treatment options.
What’s known about COVID-19 and the development of blood clots?
Normally, blood clots help stop bleeding when you’re injured. When a blood vessel is injured, it produces proteins that attract platelets and other clotting factors. These clump together to form a clot that plugs the injury and allows it to heal.
However, sometimes blood clots form in the absence of an injury. This is potentially dangerous because the clot can restrict the flow of blood within your blood vessels, leading to complications like stroke or heart attack.
Blood clots with COVID-19 have most often been seen in people who’ve been hospitalized with the disease.
A study of 184 people in the ICU for severe COVID-19 found that 31 percent Trusted Source of these individuals experienced complications related to blood clots. It’s still unknown how common blood clots are in individuals who have a mild case of COVID-19.
COVID-19 complications from blood clots can happen across all ages. A small study looked at 14 people with COVID-19 who had experienced a stroke due to a blood clot.
The study found that 42 percent Trusted Source of participants were under age 55 and had no existing risk factors for stroke.
Why can COVID-19 cause blood clots?
It’s still unclear why blood clots develop in people with COVID-19. However, a recent studyTrusted Source, published in the journal The Lancet Haematology, helps shed some light on this topic.
The study involved 68 people hospitalized with COVID-19. Of these people, 48 were in the ICU and 20 were not. Their blood was analyzed for various markers associated with clotting.
The markers in question are involved with the activation of the cells lining your blood vessels (endothelial cells) and platelets. Both endothelial cells and platelets are important for starting the clotting process.
The study found that the people in the ICU had higher levels of these clotting markers than those who weren’t in the ICU.
The exact cause of the increase in clotting markers is uncertain, but it could be due to one (or a combination) of the mechanisms below:
Endothelial cells express ACE2 protein, which the new coronavirus uses to enter cells. Because of this, the virus could directly invade and damage endothelial cells, triggering your body’s clotting mechanism.
If endothelial cells aren’t being directly infected, damage to the tissues around them due to viral infection or your immune response could cause increased clotting.
An increase in inflammatory molecules that your immune system produces in response to viral infection could activate clotting.
Another study that was published in the journal Blood supports some of the findings above.
In this study, the platelets of people hospitalized with COVID-19 were found to be hyperactive, having increased activation and aggregation (clumping).
SUMMARY
Although the exact mechanism is unclear, COVID-19 appears to cause increased activation of cells that are important in initiating the clotting process. This may lead to an increased risk of blood clots.
Are some people at higher risk for developing blood clots?
You may be at higher risk for blood clots from COVID-19 if you:
- Are hospitalized. Most cases of blood clots in people with COVID-19 have been reported in individuals who’ve been hospitalized.
- Have high levels of certain markers. A studyTrusted Source of more than 300 people hospitalized with COVID-19 found that high D-dimer levels were a strong predictor of death. Other clotting and inflammatory markers have also been associatedTrusted Source with clotting or poor outcome.
- Have other conditions that put you at risk for clotting. Some examples include heart disease, diabetes, and obesity.

What complications can blood clots cause?
Having a blood clot can lead to some potentially serious complications, such as:
Stroke: A blood clot can block blood vessels in your brain, interrupting blood flow and leading to a stroke. If a clot temporarily reduces blood flow, you can have a transient ischemic attack (TIA), or ministroke.
Pulmonary embolism: A pulmonary embolism is when a blood clot travels to your lungs and blocks the flow of blood. This can decrease oxygen levels and damage lung tissue.
Heart attack. A heart attack happens when blood flow to your heart tissue is cut off. Blood clots are a potential cause of heart attacks.
It’s also possible that a blood clot could restrict blood flow in other parts of your body, causing potentially serious damage. Some examples of other areas that a blood clot may affect include your:
- limb
- gastrointestinal tract
- kidneys
COVID-19 and capillaries
Capillaries are the smallest blood vessels in your body. They can be so narrow that red blood cells must pass through them in a single-file line.
Clots due to COVID-19 can also affect capillaries. In fact, it’s possible that the presence of tiny clots in capillaries could contributeTrusted Source to the condition known as “COVID toes.”
These tiny clots can be dangerous. Trusted Source in people with COVID-19 pneumonia, where inflammation and fluid buildup already make it difficult to breathe.
A clot in the capillaries inside the tiny air sacs of your lungs can restrict blow flow, further lowering oxygen levels.
What are the treatment options?
People who have blood clots are often treated with a medication called a blood thinner, which reduces clotting in your body. Blood thinners can help prevent existing clots from getting bigger and keep new clots from forming.
One study, Trusted Source examined the effects of blood thinners in people who were hospitalized with COVID-19. It found that people who were treated with blood thinners in the hospital had a more positive outcome than those who were not.
It’s important to note that this study was only observational and wasn’t a clinical trial.
Going forward, clinical trials will need to be performed to determine the safety, effectiveness, and proper dosage of blood thinners to treat COVID-19-related blood clots.
Is there anything you can do to reduce your risk for blood clots?
You can reduce your risk for blood clots in general by doing the following:
Stay active: A sedentary lifestyle can increase your blood clot risk, so make sure to get regular exercise. If you need to sit for a long time — like with working or traveling — try to take regular breaks so you can get up and move around.
Lose weight if you’re overweight. Shedding excess weight can help lower your risk for developing blood clots.
Don’t smoke. Smoking can damage the lining of your blood vessels and cause clots to form.
Know the side effects of medications. Some types of medications, including birth control pills, hormone replacement therapy, and certain cancer drugs, may increase your risk for blood clots. Work with your doctor to make sure these are properly managed to minimize the risk of blood clots.

The best way to help prevent COVID-19-related blood clots is by taking steps to avoid contracting the new coronavirus. The most effective way to avoid this highly contagious virus is to:
- practice physical distancing.
- Avoid people who are sick.
- Wash your hands frequently.
- Avoid touching your nose, mouth, and eyes with unwashed hands.
- Wear a face mask if you need to be around people who aren’t in your household.
If you come down with COVID-19 and are concerned about your blood clot risk, don’t hesitate to speak with your doctor.
If you’re at increased risk for blood clots, it’s possible that your doctor may prescribe an oral blood thinner medication.
The bottom line
COVID-19 can potentially cause blood clots. So far, blood clots have mostly been seen in people who are hospitalized with severe COVID-19 symptoms.
It’s unclear exactly how COVID-19 leads to blood clots. However, the infection has been found to activate cells that are involved in the clotting process.
Blood clots due to COVID-19 can lead to complications like stroke and heart attack. These can occur across all age groups and in otherwise healthy people.
If you become ill with COVID-19 and are concerned about your blood clot risk, be sure to talk with your doctor.
A coronavirus is a type of virus that can cause respiratory illness in humans and animals. In 2019, a new coronavirus called SARS-CoV-2 emerged in Wuhan, China, and quickly spread around the world.
An infection with the new coronavirus causes a respiratory disease called COVID-19.
As with most viruses, the incubation period of SARS-CoV-2 can vary from person to person. Read on to learn more about how long it may take for symptoms to develop and what to do if you think you have COVID-19.
What to know about the incubation period
An incubation period is the time between when you contract a virus and when your symptoms start.
Currently, according to the Centers for Disease Control and Prevention (CDC)Trusted Source, the incubation period for the novel coronavirus is somewhere between 2 to 14 days after exposure.
According to a recent report, Trusted Source, more than 97 percent of people who contract SARS-CoV-2 show symptoms within 11.5 days of exposure. The average incubation period seems to be around 5 days. However, this estimate may change as we learn more about the virus.
For many people, COVID-19 symptoms start as mild symptoms and gradually get worse over a few days.
How is the virus transmitted?
The CDC recommends, Trusted Source that all people wear cloth face masks in public places where it’s difficult to maintain a 6-foot distance from others. This will help slow the spread of the virus from people without symptoms or people who do not know they have contracted the virus. Cloth face masks should be worn while continuing to practice physical distancing.
Instructions for making masks at home can be found here, Trusted Source.
Note: It’s critical to reserve surgical masks and N95 respirators for healthcare workers.
SARS-CoV-2 spreads mostly from person to person through close contact or from droplets that are scattered when a person with the virus sneezes or coughs.
The novel coronavirus is highly contagious, which means it spreads easily from person to person. According to the CDC, Trusted Source, people who have the virus are most contagious when they’re showing symptoms of COVID-19.
Although it’s much less common, there’s a possibility that someone who is infected with the coronavirus can transmit the virus even if they’re not showing symptoms.
It’s also possible that the virus can be transmitted via touching virus-contaminated surfaces and then touching your mouth or nose. However, this isn’t the main way the novel coronavirus spreads.
How to protect yourself
The best way to prevent yourself from contracting the novel coronavirus is to wash your hands often.
Use soap and water and wash for at least 20 seconds. If you don’t have soap and water, you can also use hand sanitizer with at least 60 percent alcohol.
Other ways to protect yourself include the following:
- Stay at least 6 feet away from anyone who seems sick, and avoid large groups of people.
- Avoid touching your face.
- Don’t share personal items with others. This includes things like drinking glasses, utensils, toothbrushes, and lip balm.
- Wipe down high-touch surfaces like doorknobs, keyboards, and stair rails in your home with household cleaners or a diluted bleach solution.
- Wash your hands or use a hand sanitizer after touching surfaces like elevator or ATM buttons, gas pump handles, and grocery carts.
- Stay home and call your doctor if you start having respiratory issues and think your symptoms are consistent with those of COVID-19.
What are the typical symptoms?
Symptoms of COVID-19 are usually mild and develop slowly.
The main symptoms are:
- fever
- shortness of breath
- cough
- fatigue
Other less common symptoms may include:
- muscle aches and pain
- nasal congestion
- sore throat
- runny nose
- chills, which are sometimes accompanied by frequent shaking
- headache
- loss of smell or taste
COVID-19 has more respiratory symptoms than a cold, which usually causes a runny nose, congestion, and sneezing. Also, a fever isn’t too common with a cold.
The flu has similar symptoms to COVID-19. However, COVID-19 is more likely to cause shortness of breath and other respiratory symptoms.
About 80 percent, Trusted Source, of people recover from the symptoms of COVID-19 without needing any special medical treatment.
However, some people can become seriously ill after contracting COVID-19. Older adults and people with compromised immune systems are at the highest risk of developing more severe symptoms.
What should you do if you think you have symptoms of COVID-19?
If you think you have symptoms of COVID-19, stay home and call your doctor. Let your doctor know:
- what type of symptoms you have
- how severe your symptoms are
- whether you’ve traveled abroad or had contact with someone who has
- whether you’ve been around large groups of people
You may need to be evaluated if:
- your symptoms are severe
- you’re an older adult
- you have underlying health conditions
- you’ve been exposed to someone with COVID-19
- Your doctor will determine if you need testing and what type of treatment is best.
If your symptoms are mild and you have no underlying health conditions, your doctor may tell you to just stay home, rest, stay hydrated, and to avoid contact with other people.

If your symptoms get worse after a few days of rest, it’s important to get prompt medical care.
What are the other types of coronaviruses?
Coronaviruses are a certain type of virus that causes respiratory illnesses in animals and humans. Corona means “crown,” and the viruses are named for the proteins on the outside of the viruses that look like crowns.
SARS-CoV-2 is the newest type of coronavirus that’s been discovered. The source of this virus is suspected to be animals in an open-air market in China. It’s still unclear what kind of animal was the source of the virus.
Coronaviruses can cause respiratory illnesses that range from a mild cold to pneumonia. In fact, most people get some sort of coronavirus infection at some point in their lives.
Other types of coronaviruses include:
- SARS-CoV, which causes severe acute respiratory syndrome (SARS). The incubation period for SARS is usually 2 to 7 daysTrusted Source, but it can be up to 10 days in some people.
- MERS-CoV, which causes Middle East respiratory syndrome (MERS). The incubation period for MERS-CoV is between 2 and 14 daysTrusted Source, with 5 to 6 days being average.
The bottom line
Most people who develop COVID-19 start noticing symptoms within 2 to 14 days after being exposed to the novel coronavirus known as SARS-CoV-2. On average, it takes about 5 days to develop symptoms, but this may change as we learn more about the virus.
If you have symptoms of COVID-19, call your doctor for advice. Until you know what type of illness you have, stay home, and avoid contact with other people.
Jill Seladi-Schulman, Ph.D.





